There’s a lot of information in this article, so we’ll give you a quick introduction and then dive right in.
For anyone who has had difficulty finding possible solutions for alopecia areata online, don’t fret. You just discovered the most up-to-date (as of 2019) collection of alopecia areata treatments available.
In this alopecia areata treatment series, we will cover the first two types of treatment options:
- Conventional treatments ←
- Experimental treatments ←
- Natural remedies (aka folk remedies)
In the next series (coming soon), we will talk about alopecia areata treatments that focus on natural hair loss remedies and provide an answer on whether alopecia can be cured naturally without any medicine.
First, a few key points about alopecia areata treatments in general.
There are currently no FDA-approved treatments specifically for this condition; however, there are a LOT of off-label alopecia areata treatments available.
These include everything from conventional therapies recommended by dermatologist to natural home remedies for inducing hair regrowth.
Plus, numerous clinical trials and ongoing research on the baldness gene and its cure are a consistent indication that we will eventually find alopecia areata treatments that work for a wider group of people in need of hair loss treatment.
One potential example is the currently trending Brontzu lotion, which we will cover in a separate article.
(If you haven’t heard about Brotzu, it’s a hair regrowth cream that created a lot of buzz in the hair loss community for quite some time now. Especially for those who have non-scarring hair loss including alopecia areata, alopecia totalis, and alopecia universalis, this lotion is definitely something you will want to check out.)
As most of you already know, there is no single solution for each type of hair loss that works for every person. Use this list to find new things to try and be sure to let us know what works for you.
Before we start, here are important notes:
1. Applicable for different types of non-scarring hair loss (AA / AT / AU): Even though we are covering alopecia areata treatments here, most of the studies we found actually involve participants with alopecia totalis (entire scalp hair loss) and alopecia universalis (entire body hair loss including the scalp region) as well.
2. Based on all human studies: We didn’t include any hair regrowth results from studies on mice here. We specifically wanted to keep the levels of efficacy more accurate, so all of the information here is based on studies with human patients.
3. All treatments except for a few (minoxidil, etc) require a doctor’s visit: If you find a treatment listed here that you want to try, be sure to discuss it with your doctor first.
At the end of the article, you will see our summary and final thoughts on current conventional and experimental hair loss treatments.
If you want to skip to the best alopecia areata treatment, jump to our final summary section; however, we recommend reading through the entire article since we share new and interesting findings in each section.
Now, let’s start with a diagram that shows alopecia areata treatment guidelines sorted by age and severity.
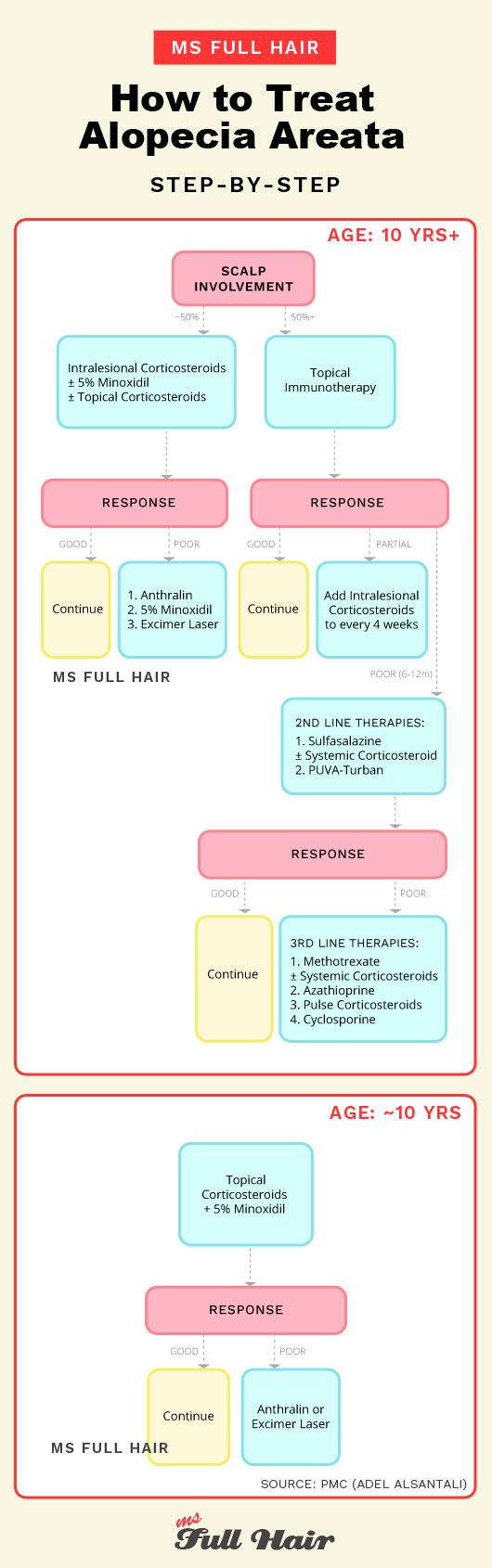
Treatments covered below:
SECTION 1 Conventional
- Corticosteroids
- 5% Minoxidil
- Anthralin
- Topical immunotherapy
SECTION 2 Experimental
- Phototherapy
- LLLT
- Immunosuppresants
- Calcineurin inhibitors
- Sulfasalazine (Azulfidine)
- Methotrexate (Trexall)
- Azathioprine (Imuran)
- Biologic agents
- PRP
- Botox
- Azelaic acid
- Carboxytherapy
- Hydroxychloroquine (Plaquenil)
- Inosiplex
- Cryotherapy
- Dapsone
- Topical Retinoids
- Simvastatin / ezetimibe
- Low-dose naltrexone (LDN)
- Topical calcipotriol
- Topical triiodothyronine
- Topical nitrogen mustard
- Prostaglandins analogs
- Imiquimod
- Stem cell therapy
Ms Full Hair final thoughts
SECTION 1
CONVENTIONAL AA TREATMENTS
This section includes a list of popularly used treatment methods (aka. conventional alopecia areata treatment).
If you go see a dermatologist for alopecia areata, these are the commonly recommended therapies (except for systemic corticosteroids).
1. Corticosteroids
The most common alopecia areata treatment
Corticosteroids, also simply known as steroids, are the most common and preferred alopecia areata treatment options prescribed by dermatologists in the last 50 years.
This powerful anti-inflammatory drug is used here to suppress the immune system from attacking its own hair follicle cells and restore its unique immune privilege.
There are several types of corticosteroids used as alopecia areata treatment:
- Intralesional corticosteroid injections (aka kenalog alopecia shots)
- Topical corticosteroid solutions (ointment, lotion, cream, gel, and foam)
- Oral and intravenous corticosteroid solutions (used as a last resort if the person is resistant to other treatments)
1.1 Intralesional corticosteroid injections
Good for mild alopecia areata
Corticosteroid shots (also known as alopecia steroid shots or intralesional steroids) are usually the first line of therapy for treating alopecia areata patients.
A small amount of corticosteroids gets injected into the upper subcutaneous layer of bald / bare patches by a dermatologist every 3-6 weeks to stimulate hair regrowth.
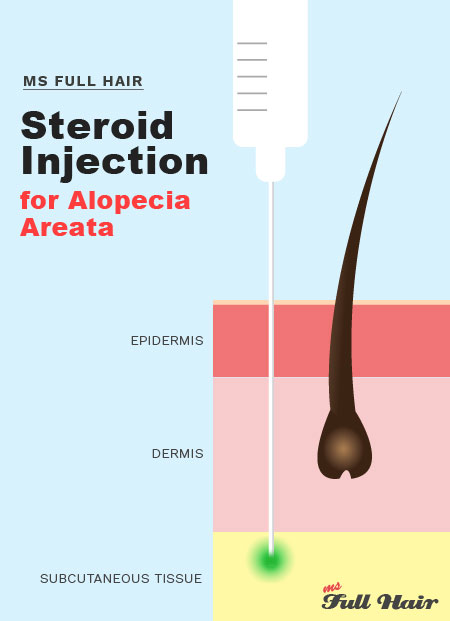
As you can imagine, this is can be a painful procedure. Thus, topical anesthetic cream is usually applied before the procedure begins.
And, this procedure is not a one-shot-per-visit deal.
Each session requires multiple triamcinolone injections into the affected area (bald patches). Each shot contains between 0.05-0.1 ml keeping 1cm distance between the injections (1).
Needle-free injection: Recently though, needle-less injection devices are gaining popularity for obvious reasons. For instance, injection devices such as PharmaJet and Porto-Jet use a narrow and precise high-pressure jet to penetrate the skin and deliver the appropriate doses of triamcinolone (kenalog).
A number of studies demonstrate promising results of using intralesional injections on alopecia areata patients.
One study (2) published in the British Journal of Dermatology reported 62% of AA participants (52 out of 84) showed hair regrowth in just 3 months after triamcinolone acetonide injections (the most widely used corticosteroid injection) compared to 7% in the placebo group.
Triamcinolone injection dose for alopecia areata: A 2011 study (3) notes that the injection dose of 10mg/ml of intralesional triamcinolone acetonide every 3 weeks resulted in 60% of participants (15 out of 25) showing hair regrowth starting by week 3.
How long does it take hair to grow back after cortisone injection?
Based on these studies, you can expect to begin seeing results in as early as 3-4 weeks.
If there is no hair growth from the steroid injections after 6 months, increasing the dosage of each injection or oral corticosteroids will often be the next recommended step by dermatologists.
Good candidate:
Intralesional steroids injection is used for mild to moderate alopecia areata (meaning patchy hair loss appearing on less than 50% of the scalp) and for patients with a shorter hair loss duration.
In general, studies indicate that intralesional injections don’t work well with severe alopecia areata, alopecia totalis and alopecia universalis.
Also, if you have had 2 years+ of alopecia areata, it may lead to poor response as well.
Alopecia shots cost:
If your health insurance company covers corticosteroid treatments (many do), your out of pocket expense is likely to be limited to your plan’s copay and deductible (check with your insurance to find out for sure). Without any health insurance, intralesional corticosteroid injection cost start from $200 per session and typically requires regular visits every 3-6 weeks.
Side effects:
The most common side effect of intralesional steroid injection is skin atrophy, in which skin thinning occurs in epidermal and dermal layers due to constant steroid exposure. This can be avoided by limiting the frequency, the amount, and paying attention to superficial injection avoidance.
Other common side effects of using intralesional steroids for alopecia areata include folliculitis (follicle inflammation) followed by spider veins appearance, temporary de-pigmentation, swelling and redness.
Highlights
- Triamcinolone acetonide (also known as Kenalog injection or triamcinolone injection for alopecia areata) is widely used for intralesional corticosteroid injections.
- Pros:
- The most recommended treatment for alopecia areata
- More effective than topical corticosteroids
- Cons
- Painful procedure
- Not everyone experiences new hair growth
- Continuous use causes decrease in scalp skin thickness (skin atrophy)
- Repeated treatment is likely to be needed to avoid relapse
- How long to see hair regrowth? About 3-6 weeks
1.2 Topical corticosteroids for alopecia areata
Topical corticosteroids – in a form of gel, lotion, cream, or ointment – is the next popular option for treating alopecia areata.
When you hear ‘alopecia areata treatment cream or alopecia lotion’, most are referring to topical steroids.
While it may not be as effective as steroid injections, corticosteroid creams are far less invasive, thus being recommended as the first therapy for children less than 10 year old (Be sure to consult your pediatrician before beginning a corticosteroid treatment on any child).
When it comes to using topical corticosteroids for alopecia areata, study results are divided.
Studies with good results:
One study shows before and after photos of a patient who used betamethasone dipropionate 0.05% (topical steroid alopecia areata cream). As you can see, partial hair growth was achieved at 3rd follow-up.
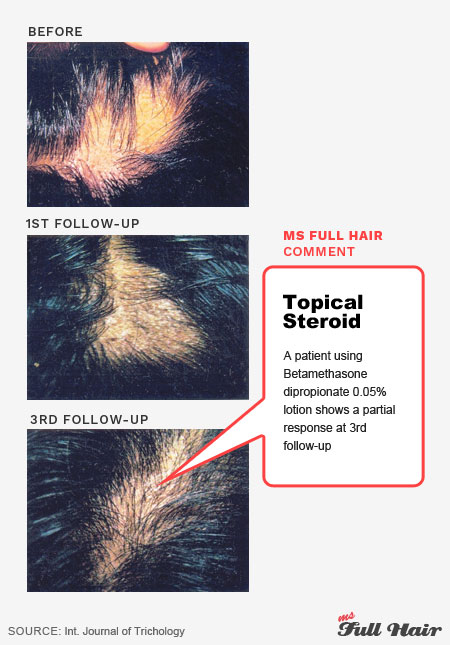
A 2003 study (4) reports that 61% alopecia areata patients experienced significant hair regrowth (more than 50% hair growth on their scalp) with 0.1% betamethasone valerate foam (a type of topical corticosteroids). On the surface, these numbers are pretty impressive.
However, the same study shows discouraging results with another group:
Studies with discouraging results:
The researchers from the same study above also tested betamethasone dipropionate lotion (topical cortisone cream used for hair growth here) to the other half of the participants. In this study, the success rate was limited to 27%.
This indicates that the type of topical steroid matters when it comes to inducing hair regrowth. In this case, betamethasone valerate foam stimulated 2.3X more hair growth than betamethasone dipropionate lotion.
Another 2003 study (5) also evaluated the efficacy of topical corticosteroids by prescribing 0.05% clobetasol propionate in 28 alopecia totalis and universalis patients.
After 6-14 weeks of application, only 30% (8 out of 28) showed hair regrowth, which is half the success rate from the previous study (61% vs 30%).
In addition, 3 out of those 8 responders experienced a relapse afterwards. In other words, the long term success rate was limited to 18% (5 out of 28).
This result also indicates and confirms a general agreement that treating alopecia totalis and alopecia universalis with topical corticosteroids alone is not effective.
Study with confusing results:
Another 2000 study (6) published in JAMA Dermatology indicates that using 0.25% desoximetasone cream resulted in complete hair regrowth in 57.6% participants, which appears to be pretty good.
Strangely enough, the placebo group had about 40% regrowth success.
The high success rate in placebo group actually makes you wonder about true efficacy of using topical corticosteroids as alopecia areata cream / lotion. In fact, it makes us wonder what else could have been contributing to this success.
What about clobetasol for alopecia areata (bald spots)?
Clobetasol propionate (brand name: Temovate) is a widely used topical corticosteroid cream for treating various skin conditions such as eczema, dermatitis, and psoriasis.
One study (7) notes that 0.05% clobetasol propionate ointment resulted terminal hair regrowth in 8 out of 28 alopecia totalis and alopecia universalis subjects. The researchers also used an occlusion with a plastic film on the scalp every night, which they believe was a contributor to the positive outcome.
Considering alopecia totalis and universalis are resistant to many other alopecia areata treatments, clobetasol propionate cream appears to be a good candidate.
Can I use rogaine with clobetasol?
According to a case report, minoxidil and clobetasol can be concurrently used together.
This case study (8) involves a man who had both androgenetic alopecia and alopecia areata (AGA and AA). The researchers note that terminal hair growth was observed in 45 days after the concurrent treatment of 0.05% clobetasol propionate cream and 5% minoxidil.
Side effects:
The most common side effect of using topical steroids is follicle infection / inflammation known as folliculitis. Folliculitis often appears after several weeks of treatment. Topical corticosteroids are needed to be used at least 3 months.
Highlights
- Out of 10 studies, 0.05% betamethasone dipropionate cream was used the most for topical corticosteroid.
- One study reports that betamethasone valerate foam stimulated 2.3x more hair growth than betamethasone dipropionate lotion (61% vs 27%).
- Pros: Less invasive than alopecia injection shots
- Cons
- Not as effective as intralesional corticosteroid injections
- Not effective for severe AA, alopecia totalis, and alopecia universalis
- How long to see hair regrowth? About 12 weeks (3 months)
1.3 Systemic corticosteroids (oral & intravenous)
For severe alopecia areata
Systemic therapy refers to internal administration of medication that spread out through the entire body.
Systemic corticosteroids are the last resort recommended for people who are recalcitrant to other alopecia areata treatment. This is commonly the case of chronic and severe alopecia areata, alopecia totalis and alopecia universalis patients.
Types of systemic corticosteroids for treating alopecia areata include:
- Intravenous or intramuscular (most common based on 41 studies)
- Oral corticosteroids (also known as oral prednisone for alopecia areata)
- Pulse corticosteroids (can be intravenous, intramuscular, or oral)
“Pulse corticosteroids” refers to a specific dosage given to a patient in a periodic manner (once a week, once a month, 3 days a month, etc), rather than everyday via an intravenous, intramuscular, or oral route.
These pulse steroids’ methods help reduce side effects of taking the medication internally for a long period of time.
A 2016 (9) review published in the Journal of American Academy of Dermatology analyzed 41 studies in total of 1078 participants and shared a number of interesting findings.
Here is the summary:
For intravenous / intramuscular pulse steroid therapy:
- 41% of patients showed more than 75%+ hair growth (ranged from 0 – 74.4% depending on a study)
- Relapse rate was 19% (ranged from 0% – 90%)
- Side effects occurred in 18% of participants
- The study with the highest success rate (74.4%) using triamcinolone acetonide, 40mg once per month via an intramascular route, but it also had extremely high relapse rate of 46.5%
- A number of studies showed 0% success rates using methylprednisolone or dexamethasone
For oral pulse steroid therapy (given monthly):
- 49% of patients showed more than 75%+ hair growth (ranged from 7.7 – 65.6% depending on a study) · Relapse rate was 19% (ranged from 7.1% – 100%)
- Side effects occurred in 31% of participants
- The study with the highest success rate (65.6%) using prednisolone 80mg 3 days a month, but the relapse rate was extremely high – 34% (more than half)
- Prednisolone was the most common form prescribed for oral steroids therapy
For mini oral pulse steroid therapy (given weekly)
- 46% of patients who showed more than 75%+ hair growth (ranged from 10 – 80% depending on a study)
- Relapse rate was 10% (ranged from 5 – 25%)
- Side effects occurred in 22% of patients
- The study with the highest success rate (80%) using betamethasone 0.1mg/kg two days a week. It had a 16.7% relapse rate, which is not that bad compared to above two therapies
To sum it up:
- Oral pulse corticosteroid therapy had the highest complete response rate (49%) on average
- Mini oral pulse corticosteroid therapy (once a week) had the lowest relapse rate (7%) on average
- Oral pulse corticosteroid therapy had the highest side effects (31%) on average
In other words, while oral pulse corticosteroid therapy had the most successful response, it also caused more side effects in participants.
Also, a number of studies note that if the duration of a disease is less than 24 months, there is higher chance of recovery.
Now, let’s focus on a specific study for a moment:
High success rate for alopecia totalis and universalis:
A 2011 (10) study published in the International Journal of Trichology demonstrated a positive result with 80% ophiasis, alopecia totalis, alopecia universalis patients experiencing hair regrowth with a combination use of betamethasone oral steroids, 1.15% anthralin topical lotion, and 2-5% minoxidil.
The study also notes that alopecia totalis and universalis patients, in which both cases are resistant to many treatments, showed cosmetically acceptable hair regrowth in HALF of the patients (4 out of 8).
Here is one of the patients who cured her baldness amazing hair regrowth results:

In addition, 2 alopecia universalis patients had a mild relapse after 12 months, which was effectively treated with intralesional corticosteroids.
While it’s difficult to pinpoint which agent contributed the most for such impressive regrowth, it showcases the fact that using multiple treatments concurrently can also result in better hair regrowth response.
Finally (and an important note), we came across many studies mentioning systemic corticosteroid therapies are not recommended for a long period of time due to the increased risk of side effects.
Side effects:
Adverse side effects of systemic (especially oral) steroids include serious weight gain and upper abdomen pain, followed by water retention, insomnia, heartburn, nausea, and anxiety.
Highlights
- If the symptom is occurring for less than a year, hair regrowth is likely to be faster
- Systemic corticosteroid alopecia areata studies with high success rates also demonstrated high relapse rates
- Predinosine is the most common oral corticosteroid
- Pros: Some studies show efficacy for treating extensive alopecia areata, alopecia universalis, alopecia totalis
- Cons: Long term treatment is not recommended due to side effects
2. 5% Minoxidil
Easy over-the-counter solution
If you are looking for an alopecia areata treatment with easy access, this is what you are looking for.
Minoxidil, also known as Rogaine, is available over the counter and thus is an easier option to consider if you are suffering from alopecia areata.
It’s one of the few FDA-approved general hair loss treatments and comes in 2% strength for women and 5% strength for men. It can be used for treating androgenetic alopecia (female / male pattern hair loss).

When using topical minoxidil for alopecia areata, the 5% strength is typically recommended for both men and women. You can also use 5% minoxidil not only for the scalp, but also for eyebrows and beard as well.
Minoxidil alopecia mechanism: Minoxidil is believed to work for hair loss by increasing blood flow to hair follicles, thus promoting steady hair growth and preventing premature hair fall-out.
One study notes that Minoxidil can be effective from 25% – 99% hair loss (meaning localized patchy hair loss to extensive alopecia areata). But, a majority of studies agree that Minoxidil is not effective for extensive hair loss including alopecia totalis or alopecia universalis.
We came across a number of interesting findings:
Dose-dependent:
One study (11) demonstrates that the effectiveness of minoxidil is actually dose-dependent.
When the researchers compared 5% and 1% topical minoxidil solutions to extensive alopecia areata participants, they observed that 5% minoxidil worked much better than 1% topical solution in terms of the quality of hair regrowth and overall response in the number of participants (81% for 5% Minoxidil vs 38% for 1% Minoxidil).
Use occlusion for maximum results:
A couple of studies (12) indicate that using occlusion after applying minoxidil helps seal the area to keep minoxidil’s active compound intact directly onto the scalp (thus increasing effectiveness). One study used petroleum jelly (Vaseline) as the occlusion method.
Use it in combination:
According to Dr. Donovan’s minoxidil alopecia areata reviews on his website, minoxidil itself doesn’t work well for stimulating new hair growth for alopecia areata (patchy hair loss) based on his experience treating many patients.
He notes that he uses Minoxidil in combination with other treatments including anthralin and DPCP for his patients.

Using minoxidil and steroid for alopecia areata: A couple of studies confirm that the use of 2% minoxidil after controlled treatment of oral prednisone (oral steroids) helps with maintaining hair regrowth.
One study (13) notes that 6 out of 7 alopecia areata participants who applied 2% minoxidil for at least 3 months as the aftercare method maintained hair regrowth after taking oral prednisone.
Side effects of minoxidil:
The main side effects of using Minoxidil for alopecia areata is contact dermatitis (itchiness, rash and redness) and hypertrichosis (abnormal hair growth over the body).
Highlights
- Using minoxidil for alopecia areata shows dose-dependent results (higher the dosage, more hair regrowth according to a study)
- Use occlusion (example: petroleum jelly) to ensure maximum application on bald patches
- Pros:
- Easy access
- You can buy topical minoxidil over the counter and try it at home
- Less side effects compared to other treatments such as corticosteroids or anthralin
- Cons:
- Minoxidil alone is not effective for alopecia totalis and alopecia universalis
- Continuous application is required
- How long to see hair regrowth? In about 3-4 months
3. Anthralin
Skin irritant to induce hair regrowth
Anthralin, also known as dithranol or drithocreme, is a topical cream used for the treatment of chronic psoriasis.
It’s a synthetic version of natural goa powder found in araroba trees and comes in cream or ointment form.
Similar to alopecia areata, psoriasis is an autoimmune condition with an increased amount of inflammation built up inside the body. The inflammation in turn causes excessive production of new skin cells.
Anthralin is used to relieve such symptoms by slowing down the production of new skin cells.
How anthralin therapy works for alopecia areata is still unclear, but scientists believe that when anthralin creates skin irritation upon topical application, it interacts and downregulates various cytokines including TNF, IL, and IFN, which are known to contribute to trigger inflammation around hair follicles.
Anthralin alopecia areata treatment:
Topical anthralin (lotion, cream or ointment) with 0.5 – 1% concentrations is currently used for alopecia areata treatment.
Topical anthralin should be applied to bald patches on the scalp with only short contact (for several minutes as a starting point and slowly building up to 1 hour) and then rinsed immediately. At least 3 months of consistent use is recommended to allow for maximum effectiveness.
One study notes that in order to increase the efficacy of anthralin therapy for alopecia areata, it requires high concentration and frequent use (everyday).
However, our findings indicate that it still may not be so effective even at high concentrations.
Comparing multiple studies that used high concentration levels (0.5 – 1%), we found that the success rates of using anthralin (dithranol) for alopecia areata were pretty low: 20-25% on average.
Mild side effects on ALL patients:
we noticed two studies pointing out the fact that all participants experienced some type of skin irritation / reaction after using dithranol. A 1987 study notes that pruritus and local erythema and scaling were seen in all patients while a 1990 study also mentions dermatitis (various types of skin irritations / inflammation).
Azelaic acid as an possible alternative:
If your alopecia areata was recalcitrant to anthralin therapy or you experienced any negative reactions, you may also want to take a look at azelaic acid. One study (15) successfully induced hair regrowth in more than half of alopecia areata participants using 20% azelaic acid cream.
Watch out for staining:
Anthralin (dithranol) cream causes yellowish-brown temporary stains on the skin (lasts several weeks before wearing off). If you have light colored hair, you may want to pay extra attention when applying anthralin onto the scalp. Wearing disposable gloves is highly recommended.
Finally, a number of studies note that topical anthralin lotion shows higher success rate when combined with other therapies including DPCP.
Highlights
- In order to be effective as alopecia areata treatment, anthralin cream should have 0.5-1% concentration and used frequently (daily)
- Success rate: about 50% for AA, 25% of Alopecia totalis
- Azelaic acid may be a good alternative option according one study
- Pros:
- Commonly prescribed by dermatologists
- May work better as a combination therapy (DPCP, etc)
- Cons:
- A high chance of developing dermatitis such as pruritus (severe itching) and local erythema (skin redness)
- Low success rate
- How long to see hair growth? 2-3 months
4. Topical Immunotherapy
High success rate, but…
Topical immunotherapy for alopecia areata acts as contact sensitizers and tricks the immune system to fight the inflammation by sending white blood cells to the area.
There are currently 2 topical immunotherapies available for alopecia areata treatment:
- Diphenylcyclopropenone (DPCP)
- Squaric acid dibutylester (SADBE)
DPCP is more favorable than SADBE because it’s affordable and more stable when in contact with acetone.
Most dermatologists try DPCP as the first topical immunotherapy for inducing hair growth. If a patient shows a poor response, then SADBE becomes the following option.
DPCP for alopecia areata – How does it work?
A dermatologist first sensitizes a small bald patch on the scalp with 2% DPCP. The patch is left with the treatment applied for the next 24 hours and then gets rinsed off.
In 1-2 weeks later, the affected spot gets analyzed to see if sensitization to DPCP has occurred. If there is a reaction, then the treatment can officially begin by starting with a very weak dose (0.0001%) and slowly increasing the concentration level as the tolerance builds up.
When significant hair regrowth (or full hair recovery) is achieved, a dermatologist usually stops the treatment or decreases the frequency of the topical immunotherapy for alopecia areata.
When DPCP is applied onto the scalp, it’s recommended to avoid sunlight for 24-48 hours as the treatment is light-sensitive.
Observation from 30+ studies:
A review of efficacy of topical sensitizers (=topical immunotherapy) for alopecia areata (16) analyzed over 30 studies.
Here are some of the observations mentioned in the publication:
- Either treatment (SADBE or DPCP) appears to produce similar hair growth results
- The overall success rate is about 50-60% (which is pretty good, especially compared to anthralin)
- However, if you look at each study, the result varies dramatically ranging from 9% to 87%
- Topical immunotherapy is not likely to be effective for extensive alopecia areata (but there are always exceptions)
- 6 months is the determination point to measure the response (if there’s no response by then, the treatment discontinues and moves on to other alopecia areata treatment)
The largest topical immunotherapy study for AA:
A Canadian study (17) analyzed total 148 participants – the largest study yet for topical immunotherapy for alopecia areata.
Let’s start with their success rates (split between “hair loss involvement:” and “success rate %”):
- Alopecia totalis and alopecia universalis: 17.4%
- Alopecia areata with 75-99% hair loss: 60.3%
- Alopecia areata with 50-74% hair loss: 88.1%
- Alopecia areata with 25-49% hair loss: 100%
Do you see a pattern?
High success rate: It shows that the efficacy of the immunotherapy treatment strongly depends on the severity of hair loss. The lower the hair loss, the better response patients had.
Here are some amazing before and after hair regrowth pictures using topical immunotherapy:
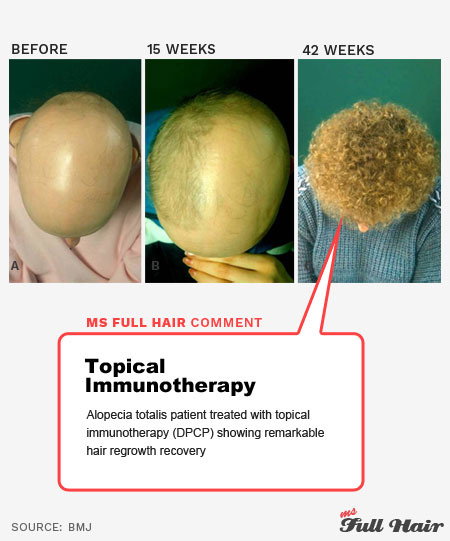
Also, significant hair regrowth started becoming visible in just 3 months.
But don’t get too excited just yet.
Followed by high relapse rate: The researchers from the study mention that there was an extremely high relapse rate of 62.6%! (Relapse happened in 2.5 years on average)
Interestingly, Medscape also notes that “almost all patients relapse” when the immunotherapy therapy discontinues.
It makes you question if it’s even worth trying the treatment in the first place.
Using immunotherapy and oral fexofenadine together:
A 2009 study (18) evaluated 121 alopecia areata subjects who had more than 50% hair loss on their scalp.
The first group received immunotherapy (DPCP / SADBE) + oral fexofenadine (brand name: allegra), while the next group only received immunotherapy.
Great for atopic alopecia areata: The study showed interesting results. Participants with atopic alopecia areata had significantly better hair regrowth by combining topical immunotherapy and oral fexofenadine (allegra) together.
However, the combined therapy didn’t make much difference in participants with non-atopic alopecia areata.
Undesirable side effects:
Also some of the common side effects reported for topical immunotherapy include lymphadenopathy (abnormal lymph nodes) in occital or cervical areas and severe dermatitis including vesicular rash, scalp swelling, hyper/hypo-pigmentation, and redness and flu-like symptoms.
For less common side effects, we found 4 studies that actually included the type of side effect in their title.
Out of 4 studies, 2 studies reported urticaria and the other 2 studies reported vitiligo while treating for alopecia areata with topical immunotherapy.
Topical immunotherapy is often recommended after corticosteroids (intralesional injections and topical solutions) are not responsive.
Highlights
- DPCP is the most common topical immunotherapy for alopecia areata
- Topical immunotherapy is often recommended when corticosteroids / steroid treatments (intralesional injections and topical) are not responsive
- Combining topical immunotherapy with fexofenadine shows greater hair regrowth response for atopic alopecia areata
- Pros: High success rate
- Cons:
- High relapse rate
- Lymphadenopathy and severe dermatitis are common side effects
- How long to see hair regrowth? About 3-6 months
SECTION 2
EXPERIMENTAL AA TREATMENTS
1. Phototherapy
Long term use may cause skin cancer
All phototherapy treatments (or light therapies) are based on using specific wavelengths of light with one purpose: Induce hair regrowth.
Some of the phototherapy methods used for alopecia areata treatments include the following.
Light therapy for alopecia areata:
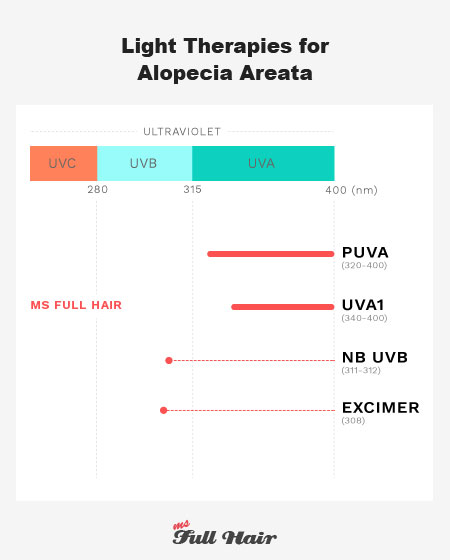
Light therapy for alopecia areata:
- PUVA (Psoralen + UVA): 320 – 400 nm (long-wavelength)
- UVA1: 340 – 400 nm (high intensity long-wavelength)
- NB UVB (Narrowband UVB): 311 – 312 nm (specific short-wavelength)
- Excimer Laser: 308 nm
1.1 PUVA
Turban based therapy shows high success rates
PUVA, also known as photochemotherapy, is an ultraviolet radiation treatment used for psoriasis, vitiligo, eczema and alopecia areata.
PUVA = Psoralen + UVA light exposure: PUVA’s P stands for psoralen, a light sensitive compound absorbing ultraviolet light and UVA is (as you already guessed it) ultraviolet radiation.
The treatment is named PUVA, as it begins with psoralen to induce high UV absorbance into a body. A patient’s scalp is then exposed to UV light to regulate certain inflammatory cell activities that are initially sensitized by psoralen.
Psoralen comes in various forms: oral consumption, topical application or even bathing the whole body into psoralen-diluted water.
PUVA alopecia areata: For treating alopecia areata, researchers have tried a variety forms of psoralen with also various success rates ranging from 6.3% – 75%. This explains why some medical reviews say a PUVA treatment is effective, while other reviews state the opposite
So is it effective or not effective?
Well, this really depends which study you are looking at.
EFFECTIVE:
A 1980 study (19) which involved 41 severe alopecia areata patients demonstrated an impressive success rate of 73% (26 out of 41 participants) experiencing hair regrowth. There were only 2 who experienced relapses in the following 6-12 months.
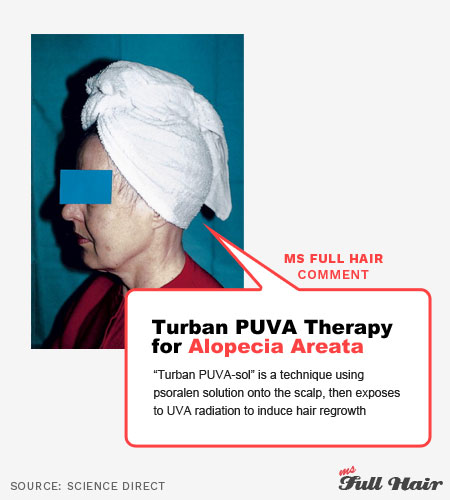
Turban PUVA for alopecia areata: Two other studies (20,21) had significant success for inducing hair regrowth in participants (67% and 75%).
Interestingly, both of these studies used PUVA turban therapy (Turban PUVASOL) instead of an oral or bathing method, which specifically distributes topical psoralen on the scalp region by using a psoralen soaked cotton towel.
NOT EFFECTIVE
But if you are looking at Dr Taylor and Hawk’s study (22), which involves 70 patients (alopecia areata, alopecia totalis and universalis) over 10 years of period, their result is completely different.
After excluding participants who experienced rapid relapse and only vellus hair regrowth (white fuzzy hairs instead of pigmented hairs), the researchers note that the success rate was only limited to 6.3% for alopecia areata, 12.5% for alopecia totalis and 13.3% for alopecia universalis patients.
However, if you look at the last sentence again, there’s something interesting about this outcome:
Hair regrowth with PUVA = AU > AT > AA
The study shows that alopecia universalis patients actually had the most hair regrowth, followed by alopecia totalis, then alopecia areata participants.
If you look at any other treatments, it’s almost always the other way around.
We also found another study that shows a similar result. With a PUVU treatment, the researchers in this study observed alopecia universalis participants had a slightly better success rate than alopecia totalis responders (55% vs 53%).
Longer the disease, the better the response:
Another interesting observation from the above 1980 study indicates that patients who had a longer period of alopecia (over 20 years) actually showed a better response than patients with more recent occurrence – which is also a contrary finding to many other treatments.
Beware of skin cancer:
The most concerning aspect of PUVA is the increased risk of skin cancer due to the cumulative exposure to ultraviolet radiation. This is why PUVA is not recommended as a long-term treatment.
Highlights:
- PUVA is not recommended as a long-term alopecia areata treatment
- Turban PUVA therapy (known as PUVASOL) shows higher success rates for stimulating hair regrowth
- Longer the disease, the better a PUVA treatment may respond for inducing hair growth
- Pro: May work well with alopecia universalis and alopecia totalis
- Con: Increased risk of skin cancer
1.2 NB UVB
Low success rate
NB UVB (narrowband ultraviolet B) is a common light therapy used for treating various skin conditions from atopic dermatitis, vitiligo, lichen planus, and others. Narrowband UVB treats various skin diseases by using shortwave ultraviolet radiation while PUVA is based on long-wavelengths.
There are only a few studies on this light therapy treatment for alopecia areata and each one shows low success rates (17-20%) for inducing hair growth.
One research even writes “The role of NB UVB in alopecia areata is questionable.”
Another research study (23) tested the efficacy of NB UVB in comparison to steroid injection for alopecia areata.
Divided into 3 groups, the first group received corticosteroid injection, the second group with NB UVB, and the last group with the combination of both.
The results were 67.5%, 17.5% and 62.5%.
In other words, NB UVB (17.5%) exhibited the lowest response when it comes to stimulating hair regrowth. To make it worse, the combined treatments of NB UVB and corticosteroid injection lowered the overall success rate than using the steroid injection alone.
Highlights
- There are only few studies on NB UVB for alopecia areata
- Every study shows low success rate
1.3 UVA1
Unclear
UVA1 (ultraviolet A-1) is a newer type of phototherapy using a high intensity and long-wavelength of 340-400 nanometers.
As UVA1 has longer wavelengths than UVB, it’s capable of penetrating deeper into the skin, thus more effectively suppressing abnormal interactions of immune cells around hair follicles.
UVA1 is used to treat a vast number of chronic skin disorders including eczema (atopic dermatitis), mastocytosis, scleroderma, morphoea, and cutaneous T cell lymphoma.
However, similar to NB-UVB, there are too few studies on UVA-1 as an alopecia areata treatment or any other hair loss disease.
One study (24) we found included 22 alopecia areata participants. Via biopsies, the researchers observed multiple positive outcomes including the absence of inflammation, increase of anagen hairs (hair growth stage), and decrease of telogen hairs (hair resting stage) in some of the patients.
Additional studies with larger sample groups are needed to find out the true efficacy of UVA1 for alopecia areata.
Similar to any other UV light therapies, skin cancer and skin aging are the big concern.
The same study as above notes that xerosis (dry skin) was observed in all patients and some experienced mild hyperpigmentation.
Highlights
- More studies are needed to validate the effectiveness of UVA-1 for treating alopecia areata
1.4 Excimer laser therapy
Positive results
If you are considering a light therapy for alopecia areata, Excimer laser therapy is something worth paying extra attention to.
Excimer laser therapy (xenon chloride excimer laser) is a targeted light phototherapy.
Using a very specific wavelength UVB light (308 nanometer), it has been effectively used to treat various skin conditions including psoriasis, vitiligo, psoriasis, atopic dermatitis, folliculitis, lichen planus, mycosis fungoides , as well as alopecia areata.
Excimer laser has a number of advantages over other phototherapies:
- Time: It requires a short amount of exposure time
- Accuracy: The light is directly targeted at the exact spot of the skin
- Exposure: it requires lower UV dose exposure
Excimer laser alopecia areata therapy: The treatment induces T cell apotosis (T cell death), thus believed to be effective in alopecia areata, T cell-mediated hair loss symptom.
Decent success rates using 308-nm excimer laser therapy in alopecia areata:
Out of 10 excimer laser treatment studies we found, 4 studies showed significant hair growth in ALL patients (even though the number of participants was fairly small in each study).
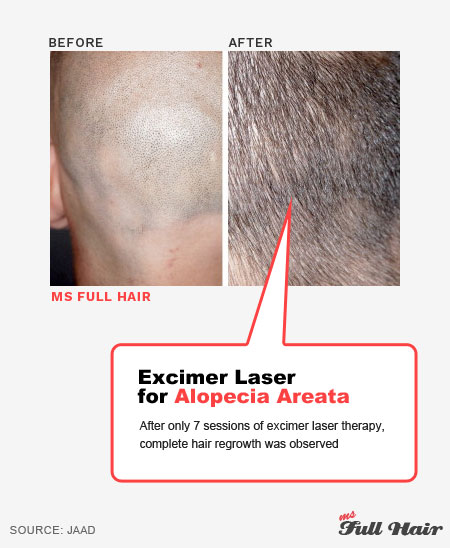
One of the 4 studies actually demonstrated interesting results: While alopecia areata participants showed 100% response to the treatment, the excimer laser didn’t have any effect for alopecia universalis or totalis.
Other studies showed a similar discouraging response for alopecia universalis or totalis, except for one Japanese study published in the Journal of Dermatology in 2016.
The researchers from this study (25) observed terminal hair regrowth in 4 out of 11 alopecia universalis patients – the most severe hair loss resistant to many other treatments. The participants were treated with the 308-nm excimer light twice a week and it required about 30 sessions to induce satisfactory hair regrowth.
Common side effects include erythema and hyperpigmentation but in a mild form.
Highlights
- Excimer laser has effectively treated various skin conditions
- Excimer laser can also possibly be an effective alopecia areata treatment according to multiple studies
- Pro: Multiples studies show high success rates for treating alopecia areata with excimer 308-nm laser
- Con: The treatment doesn’t appear to be effective for alopecia totalis and alopecia universalis
2. Low-Level Laser Therapy (LLLT)
Only 2 studies, but very promising
The HairMax LaserComb (or a laser cap) may be the first thing that comes to your mind when you think about low-level laser therapy (LLLT).
While LLLT is more known for treating androgenetic alopecia, these 2 studies suggest that it may also work for alopecia areata as well.
Very promising result of using low level laser therapy for alopecia areata:
There are only two studies on LLLT for the treatment of alopecia areata, but both showed significant responses.
STUDY 1:
The researchers (26) investigated how pulsed diode laser therapy (904nm) works for AA patients. 16 patients were involved and most of them had multiple bald patches on their scalp. In order to increase the accuracy of the result, one of the patches from patients with multiple bare spots was left without an treatment (thus a control patch)
Now, the best part: 32 out of 34 patches (94%) showed hair regrowth, while control patches didn’t have any hair growth.
STUDY 2:
A 2014 study (27) evaluated the efficacy of low level laser therapy as alopecia areata treatment using a similar method as above. One of the bald patches on each patient was left without treatment for comparison.
There were total 52 bare patches (29 active and 23 control patches) among 23 participants.
After receiving 3 sessions per week just over one month, significant improvement was observed in before and after hair count, compared to placebo patches.
But, don’t get too excited thinking you are going to buy a HairMax just yet!
Unfortunately, wavelengths between HairMax and the devices used in the studies are completely different. To be specific, HairMax uses 655 nm wavelength while the laser devices used for the alopecia areata studies had 905 nm.

Also, there are only 2 studies on this right now (at least, that’s all we were able to find). In order to find out the true efficacy of this treatment, more studies with large samples will be needed.
Laser treatment for hair loss side effects:
Mild side effects such as itching, scaling and erythema (skin redness and swelling) were noted as the device was in contact with the skin.
Highlights
- Low level laser light therapy (LLLT) shows high success rates for treating alopecia areata but there are only 2 published studies exist
- Pro: both studies show significant improvements on hair regrowth without any major side effects
- Cons: More studies are needed
3. Immunosuppressants
3.1 Calcineurin inhibitors for alopecia areata
Calcineurin is a protein enzyme that activates T cells and upregulates the expression of IL-2 (interleukin 2). Calcineurin inhibitors are used to modulate inflammation by blocking abnormal activities of T cells.
3 Calcineurin inhibitors are used as possible alopecia areata treatment methods:
- Cyclosporine (oral or topical): Promotes significant decrease in the CD4/CD8 T cell ratio
- Tacrolimus (topical): Reduces IL-2 production
- Pimecrolimus (topical): Prevents Th1 and Th2 cytokine synthesis
Cyclosporine – Be aware of relapse
Cyclosporine is an immunosuppressive drug that comes in an oral or topical form. Both forms work by blocking T cell proliferation and interferon-y production.
Topical cyclosporine not so effective for alopecia areata:
Unfortunately, cyclosporine hasn’t shown any significant efficacy for promoting hair regrowth when used as a topical solution, even after 12-months of consistent treatment in one study.
Using oral cyclosporine in the treatment of severe alopecia areata:
Multiple studies show that oral cyclosporine is either prescribed alone or in combination with oral steroid (corticosteroid).

Most studies with oral cyclosporine (or with oral corticosteroid) show hair regrowth responses. A couple of studies even note that ALL of their participants responded to the treatment (29,30).
High success followed by high relapse (baldness):
But there is a caveat – As soon as the cyclosporine treatment discontinued, almost all patients in those 2 studies experienced lost all of their hairs again regardless of severity of alopecia areata.
Side effects:
Some of the side effects of oral cyclosporine include headache, abnormal body hair growth, tremors, upset stomach. For severe side effects, high blood pressure and kidney damage may occur.
Highlights
- Oral cyclosporine is often prescribed with oral corticosteroid as alopecia areata treatment
- Pro: Oral cyclosporine showed some effectiveness resulting in hair regrowth
- Con: A relapse will likely to occur upon the discontinuation of the cyclosporine induced hair growth treatment
Tacrolimus – Not so effective
Tacrolimus is also a calcineurin inhibitor with an immunosuppressive property.
Role of tacrolimus:
While oral tacrolimus is used to prevent the body from rejecting organ transplant, a topical form of tacrolimus is used for treating atopic dermatitis (eczema).
Using topical tacrolimus for alopecia areata doesn’t seem so promising.
A 2005 study notes that no terminal hair growth was observed after treating alopecia areata participants with tacrolimus ointment for 24 weeks.
Another study also states that the success rate was only 4%.
Side effects include itching, burning sensations, and stinging during initial treatments. It can also cause flu-like symptoms, muscle pain and headache.
Highlights
- Tacrolimus ointment shows little to none benefit for inducing hair regrowth
Pimecrolimus – Low success rate
Also known as Elidel (brand name), pimecrolimus has immunosuppressive and anti-inflammatory properties and is used for treating atopic dermatitis with a topical application.
When it’s used as an alopecia areata treatment results somewhat vary, but seem to be more on the ineffective side.
Using Elidel cream for alopecia areata:
A 2014 study (31) with 80 alopecia areata participants tested the efficacy of topical pimecrolimus by dividing them into two groups: Elidel group and the Elidel (topical pimecrolimus) + tretinoin (topical retinoid medicine) group.
Combined therapy works better:
Complete hair regrowth was observed in 45% of Elidel + tretinoin group participants, while it was 20% in Elidel only.
The result makes it clear that topical pimecrolimus can be more potent for inducing hair regrowth, when it’s combined with other treatment (Elidel + tretinoin in this case).
Side effects: Side effects include burning, itching, tingling, muscle pain, flu like symptoms (cough, runny or stuffy nose), diarrhea, and eye irritation.
Highlights
- One large study indicates that pimecrolimus (Elidel) cream is more effective for inducing hair regrowth on alopecia areata patients when used with topical tretinoin (topical retinoid)
3.2 Sulfasalazine
Somewhat effective, but has side effects…
Sulfasalazine (brand name: Azulfidine) is an immuno-suppressive and inflammatory oral medicine used for treating ulcerative colitis, Crohn’s disease, rheumatoid arthritis, inflammatory bowel disease and other types of autoimmune diseases including severe alopecia areata.
Response rate: The average response rate of using sulfasalazine for alopecia areata is 50% and above. But when you look at significant hair growth, the number reduces to about half – 25%.
Sulfasalazine for alopecia universalis and alopecia totalis:
A 2012 study (32) evaluated the effectiveness of sulfasalazine in alopecia areata, alopecia totalis and alopecia universalis participants.
The researchers observed that 23% of participants experienced hair regrowth. Among the subjects who responded to sulfasalazine, 80% had localized alopecia areata, while the remaining 20% had either alopecia totalis or universalis.
One review journal also notes that sulfasalazine is dose-dependent, thus continuous treatment will likely be needed to sustain hair regrowth from the medicine.
Expect side effects:
One study (33) notes that 7 out of 22 participants, which is about 30%, experienced minor side effects including gastrointestinal distress and headache.
The World Health Organization published a document in 2009 showing that 25% of people experienced some type of adverse effects. Some of these side effects included rash, vomiting, itching, nausea, loss of appetite, weight loss, and headache.
Highlights
- Significant hair regrowth was seen in about 25% participants who took sulfasalazine for persistent / recalcitrant alopecia areata, according to two studies
- Sulfasalazine also induced hair regrowth in small subset of alopecia universalis and alopecia totalis subjects
- Continuous treatment is likely to be required to avoid relapse
- The occurrence of side effects is high
3.3 Methotrexate
Taking folic acid is a must
Methotrexate (brand name: Trexall) is another immunosuppressant drug used to treat cancer, autoimmune diseases such as rheumatoid arthritis, and skin conditions such as psoriasis.
Methotrexate and folic acid:
Methotrexate is a folic acid antagonist. This means that methotrexate blocks the enzyme called dihydrofolate reductase, which results in folate deficiency. Thus, taking folic acid supplement is a must when you are under Methotrexate for treating alopecia areata or other diseases.
Great result with oral corticosteroid:
A couple of studies (34) indicate that using methotrexate in combination with oral corticosteroids (steroids) stimulated significant hair regrowth in about 65% of alopecia areata, alopecia totalis, and alopecia universalis participants (with more than 50% hair regrowth on the scalp).
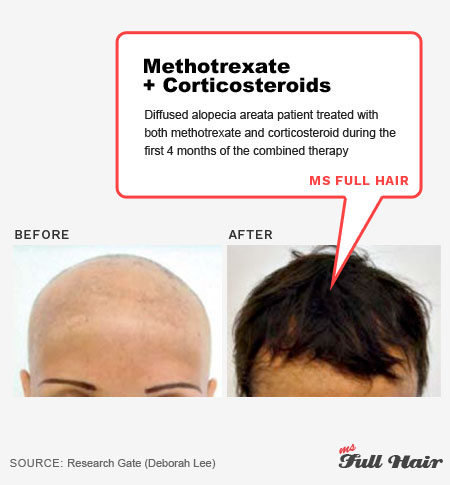
Using Methotrexate alone also showed a great response in 58% of alopecia areata participants (8 out of 14) in one of the studies.
Relapse happens:
Unfortunately, relapse was also unavoidable. One study notes that 80% of participants who were treated with methotrexate and oral corticosteroid experienced a relapse.
This indicates that continuous treatment is required to maintain hair regrowth.
Methotrexate induced alopecia
Can methotrexate also cause alopecia? Ironically, one of the side effects of methotrexate (MTX) appears to be hair loss. We came across multiple people on MTX for other diseases experiencing noticeable hair loss.
Luckily, a number of people note that excessive shedding will gradually subside upon reduced dosage or discontinuation of the medication.
Side effects:
Common side effects of methotrexate(other than hair thinning) include elevated transaminases (elevated liver enzymes), vomiting, nausea, shortness of breath, headaches, diarrhea, mouth sores, and fever or chills.
Doctors note that some of these side effects can be prevented by taking folic acid (1mg of folic acid everyday or a single 5mg once a week – depending on a physician).
Highlights
- Taking a folic acid supplement is a must as Methotrexate is an anti-folic agent
- Methotrexate induces significant hair regrowth in alopecia areata, alopecia totalis and alopecia universalis according to a number of studies (but a relapse seems unavoidable)
- Ironically, methotrexate appears to induce diffused hair thinning according to people who were taking the medication for other purposes
3.4 Azathioprine
Induce hair loss or hair regrowth?
Azathioprine (brand name: Imuran) is an immunosuppressive drug used for organ transplants and autoimmune disease such as rheumatoid arthritis, Crohn’s disease, ulcerative colitis and others.
Cause of hair regrowth or hair loss?
You may want to think twice if you are considering to take azathioprine for alopecia areata.
Hair regrowth: One study (35) presented significant hair regrowth for alopecia universalis with a 43% success rate, even though one third of the patients experienced a relapse afterwards.
Another study (36) also showed 52.30% response rate treating alopecia areata patients.
Azathioprine (Imuran) induced alopecia: However, another study observed that azathioprine caused alopecia totalis in a patient who was taking the drug for vitiligo.
She experienced dramatic hair loss just in 15 days of taking the drug and eventually, all of her hair was gone. Interestingly, during hair loss, an extremely low blood count was observed, in which the physician believes as a possible reason of why Imuran causes hair loss.
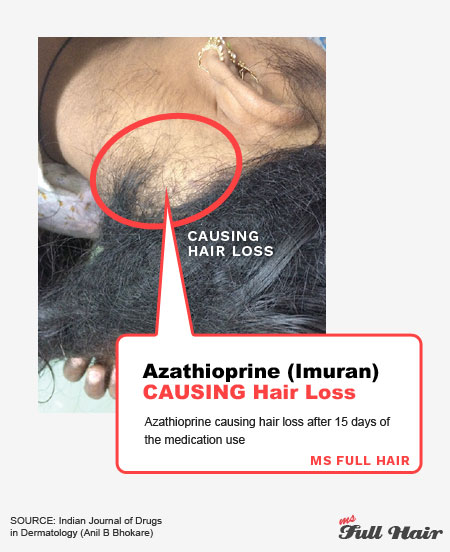
Is hair loss from Imuran permanent? The same study notes that once azathionprine discontinued, her hair started growing again.
Side effects
Side effects of azathioprine (Imuran) are similar to other immunosuppressant medicines which include vomiting, diarrhea, decrease in appetite, skin rash and hair loss.
Highlights
- Studies show that Azathioprine (Imuran) may induce hair regrowth OR the cause of alopecia
4. Biologic agents
Unlike immunosuppressive drugs that suppress the immune response at multi-levels, biologic drugs target a specific immunosuppressive action(s), which in turn increases effectiveness and result in less adverse side effects.
The table below shows a list of cells and cytokines that trigger alopecia areata due to abnormal activities.
Alopecia areata (AA) triggers and its inhibiting medicine / drugs:
| Elevated in AA | Drug (Inhibitor / Modulator) | Brand name | Note |
|---|---|---|---|
| T cells (CD4, CD8) | Ruxolitinib | Jakafi | JAK inhibitor |
| Tofacitinib | Xeljanz | JAK inhibitor | |
| Baricitinib | Olumiant | JAK inhibitor | |
| Abatacept | Orencia | T cell proliferation reduction and reduce inflammatory cytokines | |
| Infliximab | Remicade | TNF inhibitor (Not effective) | |
| Adalimumab | Humira | TNF inhibitor (Not effective) | |
| Etanercept | Enbrel | TNF inhibitor (Not effective) | |
| Alefacept | Withdrawn | ||
| Efalizumab | Withdrawn | ||
| CYTOKINES: | |||
| IL-1 | |||
| IL-2 | Aldesleukin | Proleukin | A recombinant (lab made) IL-2 molecule with immunomodulatory properties (Not effective) |
| IL-9 | |||
| IL-4 & IL-13 | Dupilumab | Dupixent | IL-4 & IL-13 blocker / Th2 inhibitor |
| IL-13 | Tralokinumab | IL-13 blocker | |
| IL-15 | |||
| IL-17 | Secukinumab | Cosentyx | IL-17 inhibitor |
| IL-23 | Ustekinumab | Stelara | IL-12 & IL-23 blocker |
| IFN-y | NI-0501 (Code name) | Anti IFN-y | |
| MIF | |||
| OTHER: | |||
| PDE4 | Apremilast | Otezla |
Using biologics agents for alopecia areata are still new compared to conventional treatments.
While a number of studies for each drug are still limited at the moment, most of the latest research on alopecia areata are focused in this field. You will see an increasing number of studies coming out from biologics in the future.
4.1 JAK Inhibitors
Emerging potential therapy
JAK inhibitor and alopecia areata: A couple of years ago, there was huge news about a discovery of a Jak kinase (JAK) inhibitor for reversing hair loss in a person who appeared to have a very severe form of alopecia areata.
The researchers from the study discovered that Ruxolitinib (brand name: Jakafi), a type of JAK inhibitor, decreased the levels of inflammatory cells (reaction of CD8+ and NKG2D+ T cells) not only in the scalp, but also in blood levels.
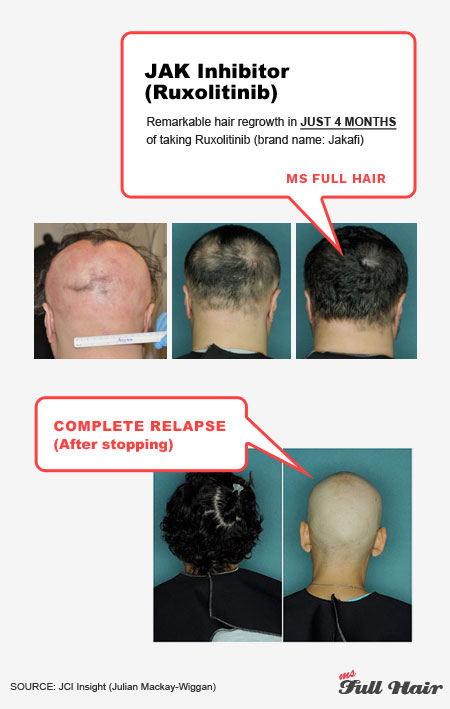
Short happy ending: Unfortunately, the happy ending didn’t last so long. When the patient discontinued the treatment, he lost all of his hair again. In order to maintain his regrowth, he had to take Xelianz on a regular-basis.
This drug dependency raises some important questions: What’s the right dosage of JAK inhibitor for alopecia areata? How often should I take? Any long term side effects?
Currently, increases in cholesterol, rare skin cancer, diarrhea, headache, lymphoma, acne, headache, and abdominal pain are some of the known side effects of taking JAK inhibitors.
Comparison of JAK inhibitors:
There are 3 Janus kinas inhibitors (JAK) currently used for alopecia studies:
- Tofacitinib (brand name: Xeljanz): Inhibits JAK 1 and JAK 3
- Ruxolitinib (brand name: Jakafi) : Inhibits JAK 1 and JAK 2
- Baricitinib: Inhibits JAK 1 and JAK 2
Xelianz alopecia areata studies and promising results: A 2016 study (38) enrolled 66 patients with severe alopecia areata. The participants were administered oral tofacitinib (Xeljanz) twice a day. After 3 months, 32% of participants had more than 50%+ regrowth, 32% had between 5-50% improvement.
A 2017 study (39) used oral tofacitinib in 90 alopecia areata patients with great results. 65 out of 90 patients responded to the therapy and 60% of the responders achieved more than 50%+ hair regrowth between 4-18 months.
Another 2017 study (40) also tested oral tofacitinib (Xeljanz) in 13 alopecia areata patients. 9 out of 13 participants experienced significant hair regrowth without any serious adverse effects.
While there are still many unknowns using a JAK inhibitor for alopecia areata, the results from most studies seem promising.
Highlights
- JAK inhibitors show promising results in inducing hair regrowth on severe forms of alopecia areata, alopecia totalis and alopecia universalis
- More research studies are on its way for optimum long lasting results
4.2 TNF Inhibitors
Paradoxical result
TNF-a (tumor necrosis factor alpha) is an inflammatory cytokine that’s shown significantly elevated in people with alopecia areata.
It would appear obvious that lowering TNF levels may result in a reverse of alopecia areata, thus multiple studies have experimented with TNF inhibitors.
The 3 most popular TNF Inhibitors used in the studies include:
- Infliximab (brand name: Remicade)
- Adalimumab (brand name: Humira)
- Etanercept (brand name: Enbrel)
Scary outcome:
Unfortunately, a TNF inhibitor actually made symptoms worse. And, in some cases, the treatment even caused new bald spots in patients who originally didn’t have any.
Here is one of the Infliximab (Remicade) induced hair loss photos:
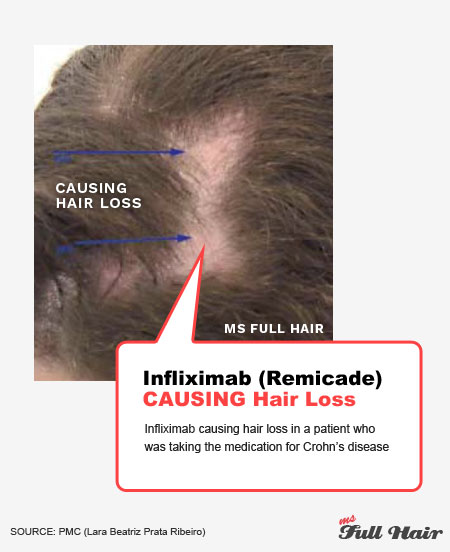
Remicade causes patchy hair loss: Several studies (41,42) note that patients who were on Remicade for Crohn’s disease experienced alopecia areata. Luckily, they had recovery upon discontinuation of Remicade (infliximab).
Almost all studies agree that TNF inhibitors are NOT likely to be effective for treating alopecia areata.
Highlights
- TNF inhibitors is NOT an effective alopecia areata treatment
- Several studies report that Remicade (infliximab) induced alopecia areata
4.3 Abatacept (T cell blocker)
Results unknown
Abatacept (brand name: Orencia) is a fusion protein that prevents T cells from full activation and reduces inflammatory cytokines including IL-2, TNF-a and IFN-y.
The drug has been effectively used for rheumatoid arthritis, but there are no clear indications for treating alopecia areata.
Out of the 3 enrolled studies we found from the Clinical Trials government directory, 2 studies were withdrawn due to funding issues. 1 study shows that the estimated completion date was July 2017, but there is no published result as of now.
Highlights
- The efficacy of using abatacept for alopecia areata is unknown
Alefacept & Efalizumab – Withdrawn from the market
Alefacept was the first biological drug approved for treating chronic plaque psoriasis.
It works by preventing CD4 and CD8 T cells from binding to antigen-presenting cells. While alefacept was FDA approved for psoriasis (which have similar inflammatory cell reactions as alopecia areata), the drug was later withdrawn due to low efficacy.
There are only two studies (43,44) we were able to find and one of them involved only 1 participant.
While the 1 participant study showed significant hair regrowth response in a woman with alopecia universalis, the sample size still seems too small.
The other study which involved 45 severe alopecia areata participants notes that the response was similar to a placebo group, thus concluded as NOT effective.
Efalizumab is an immunosuppressant biological drug. It was withdrawn from the market due to severe side effects including a fatal brain disorder. When tested for alopecia areata, it didn’t show any benefit.
Highlights
- Alefacept and Efalizumb are not effective and were withdrawn from the market
4.4 Aldesleukin (Lab made IL-2)
Partial hair growth
Aldesleukin (brand name: Proleukin) is a recombinant interleukin 2 (this simply means lab-made interleukin-2). It’s an immune-modulating protein that regulates activities of T and B lymphocytes.
A 2014 study (45) published in JAMA Dermatology reports partial hair regrowh was observed in 80% of patients (4 out 5) after treating them with low-dose IL-2.
The researchers also didn’t observe any adverse effects.
While the participants didn’t have full hair regrowth, the high response rates with no side effects makes low-dose IL-2 a good candidate for future alopecia areata treatment.
Highlights
- Aldesleukin (recombinant interleukin 2) shows high response rates and no side effects in one study
4.5 Dupilumab
2 Contradictory case reports
Dupilumab (brand name: Dupixent) is a prescription biologic drug used for treating atopic dermatitis (eczema) with great results.
Dupilumab inhibits Th2 cells by blocking interleukin-4 (IL-4) and interleukin-13 (IL-13). Blocking these interleukins helps relieve atopic dermatitis.
Interestingly, a number of studies note that alopecia areata can also be treated by inhibiting overactive Th2 cells.
Dupixent and alopecia areata: There are currently two published case reports on Dupilumab as alopecia areata treatment. The results from each study are so different that it creates some confusion.
Case #1: Dupilumab (dupixent) cured alopecia areata
This case study involves a girl with atopic dermatitis and alopecia totalis, in which both symptoms lasted more than 10 years.
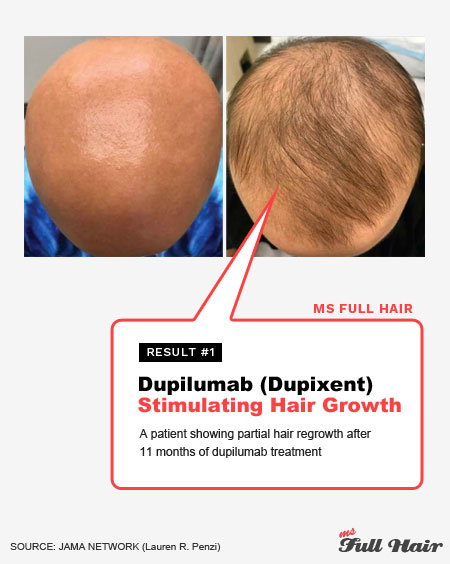
After 6 weeks of dupilumab injections, the researchers noticed not only significant improvement in her eczema, but also white fuzzy hairs sprouting out on her scalp.
In 9 months, 60% of her scalp was covered with thick pigmented hairs and by 11 months, there was considerable hair regrowth.
Case #2: Dupilumab (dupixent) caused alopecia areata.
A male patient who was also taking dupilumab for atopic dermatitis noticed something unusual on his scalp: patchy hair loss.
While his eczema condition improved, his hair loss became easily noticeable under dupilumab. In order to reverse alopecia areata, he had to be treated with steroid injections.
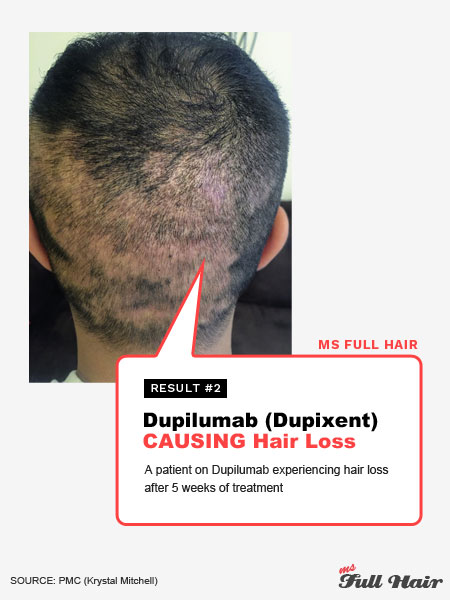
Both case studies show completely different results, so finding the true efficacy of using dupilumab for alopecia areata seems uncertain.
There is currently a clinical trial ongoing (started early2018). This dupilumab study involves 54 subjects with alopecia areata. Hopefully, the result will help shed some light (we will keep you updated with the result – make sure to sign up for our newsletter to get updates).
Side effects of dupilumab:
Dupilumab may cause eye-related side effects such as dry eye, eye itching, cornea inflammation and pink eye.
Highlights
- The efficacy Dupilumab is confusing as studies show contradictory results (hair regrowth vs hair loss)
4.6 Tralokinumab
Under investigation
Tralokinumab is also a Th2 blocker that specifically targets interleukin-13 (IL-13 – one of the main cytokines shown upregulated in alopecia areata scalp).
There’s one pilot study (46) of tralokinumab for alopecia areata with a completion date marked for last year, but no results have been posted yet.
Highlights
- Using tralokinumab for alopecia areata is under clinical trial right now
4.7 Secukinumb (IL-17 inhibitor)
Unexpected discovery
Secukinumab (brand name: Cosentyx) is an interleukin-17 (IL-17) inhibitor used to treat plaque psoriasis, psoriatic arthritis, and ankylosing spondylitis.
Secukinumab and alopecia areata: Unfortunately, 2018 study indicates that secukinumab is not effective as an alopecia areata treatment.
Out of 7 participants who were treated with secukinumab (Cosentyx), only 1 participant (14.3%) had partial hair regrowth in one study (47). The rest either showed no change or had increased hair loss as a side effect of Cosentyx.
Something unexpected:
One case study had an interesting discovery while treating a patient with secukinumab for psoriasis.
The patient experienced his hair turning grey in his early years and also had androgenetic alopecia.
After 6 months of the treatment, he noticed that his grey hair started turning back to the original brown color, but it didn’t stop there. New hairs were found filling up the thinning spots all over his scalp.
Here are the before and after photos:
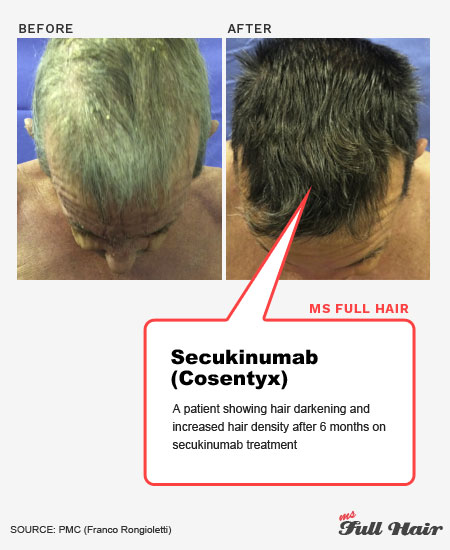
Based on this study, it appears that secukinumab may work better for pattern hair loss than alopecia areata; however, since there was only 1 participant in the case report, more studies will be needed to find out the true efficacy of using cosentyx for different types of hair loss.
Highlights
- Secukinumb is not effective inducing hair regrowth for alopecia areata according to a study
- One case report indicates that it may work for androgenetic alopecia and reversing premature hair greying
4.8 Ustekinumab (IL-23 Inhibitor)
May induce NEW patchy hair loss
Ustekinumab (brand name: Stelara) is a FDA approved drug used for the treatment of chronic / severe plaque psoriasis. It works by inhibiting interleukin 12 and interleukin 23 (both interleukin levels are also elevated in alopecia areata).
Study results divided:
Ironically, study results are divided far left and far right.
Hair growth: Out of the 6 studies we found, 4 reported excellent response rates of hair regrowth using ustekinumab; however, the other 2 studies share a very concerning result: induced patchy hair loss.
Hair loss: The participants from these 2 studies (48,49) were under ustekinumab (Stelara) for treating moderate to severe psoriasis. While all of them achieved great improvement for psoriasis, they ALL experienced severe patchy hair loss while on Stelara.
Once again, such divided results raise some concern of using Stelara for treating alopecia areata.
Highlights
- Depending on which study you are looking at, ustekinumab either induces hair regrowth or hair loss
4.9 IFN-γ Inhibitor
Significant regrowth on AA, but only 1 study
Multiple studies show that serum levels of IFN-γ (interferon-gamma) are significantly elevated in alopecia areata, alopecia totalis and alopecia universalis than people without non-scarring hair loss.
There is only one biologics study on anti IFN-y in regards with treating alopecia areata.
In this study (50), the researchers observed significant hair regrowth on most participants with progressive alopecia areata (8 out of 9). In addition, 3 out of 5 alopecia totalis or universalis participants responded to the treatment, but limited with partial terminal hair growth.
Highlights
- Anti IFN-y shows the most effective response in early intervention of hair loss
4.10 Apremilast
Remarkable for psoriasis-induced alopecia areata
Apremilast (brand name: Otezla) is a PDE4 (phosphodiesterase 4) inhibitor used for treating psoriasis and psoriatic arthritis.
PDE4 inhibitors work by reducing pro-inflammatory cytokines including IFN-y, IL-17, IL-22, and TNF. These cytokines are significantly increased in the scalp regions of alopecia areata patients, thus making their reduction a potential candidate for hair loss treatments.
3 different results of using Apremilast (Otezla) for alopecia areata:
Result #1: One study (51) with 9 participants observed no benefits of using Apremilast as alopecia areata treatment.
Result #2: Another study (52) notes that Apremilast (Otezla) worked for inducing hair regrowth in an alopecia totalis patient. But when we looked at the before and after photos, the result was far from cosmetically acceptable.
Result #3: The last study (53) actually had a remarkable outcome of using Apremilast – FULL hair regrowth. But there was one big difference among the patients from the other studies: this participant had alopecia areata along with plaque psoriasis on her scalp.
After 12 weeks of Apremilast treatment, both of her symptoms (psoriasis and alopecia areata) were totally gone.
What do these results mean?
The last study proves that Apremilast indeed works wonders for treating psoriasis. If psoriasis was what caused her alopecia areata in the first place, the remarkable result makes sense as the drug effectively corrected the underlying symptom (psoriasis).
The results from the other two studies (no benefit and limited hair regrowth) indicate that Apremilast may not be an effective treatment for non-scarring alopecia areata, even though it contains multiple pro-inflammatory blocking properties.
Highlights
- Apremilast effectively treated psoriasis alopecia areata in one study
- Apremilast shows none to minimal results for regular alopecia areata participants in two studies
5. Platelet-rich plasma (PRP)
Promising (and pricey)
Platelet-rich plasma (PRP) treatment works by stimulating the body by using a patient’s own blood to produce new cells, thus encourage healing.
PRP was successfully used in androgenetic alopecia (pattern hair loss) in a 2014 study with a significant increase in hair counts.
Since then, many studies have also applied the PRP treatment for alopecia areata patients with positive outcomes in most cases.
High response rates:
A 2013 controlled study (54) shows that participants who were treated with PRP had significantly greater hair regrowth compared to the triamcinolone acetonide (steroid injection) group.
Another study (55) involving 30 progressive and chronic alopecia areata subjects also observed 21 of them (70%) having noticeable hair regrowth after the PRP treatment.
Here are PRP before and after hair regrowth photos for treating alopecia areata from another study:
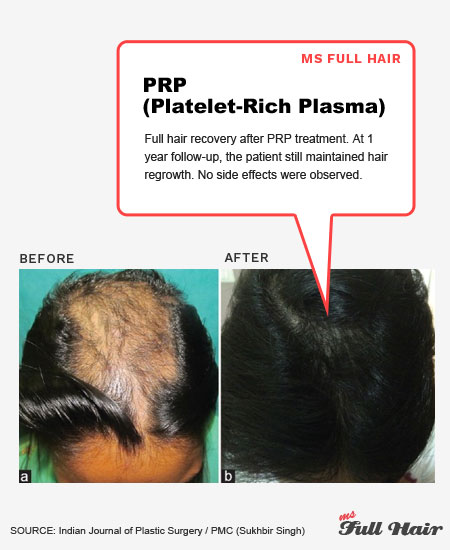
One caveat – PRP for hair loss cost:
While the platelet-rich plasma treatment seems promising, the cost is high. The PRP injection ranges from $500 to $2000 making it expensive as a regular treatment.
Highlights
- Multiple studies show positive results, but the treatment cost is high
6. Botulinum Toxin (Botox)
0% Success in 1 study
Using botox for alopecia areata doesn’t seem to be a good idea according to some studies.
A 2010 study (56) experimented with Botulinum Toxin type A by injections on 7 patients.
One participant dropped due to severe aggravation and the rest didn’t see ANY hair regrowth. The researcher concludes that botox “cannot be used” for treating alopecia areata.
May induce hair loss:
Another study (57) makes it more worrisome about using Botox: 5 patients received periodic Botox injections for their forehead wrinkles; however, ALL of them noticed their frontal hair loss becoming increasingly evident after repeated injections.
The last study (58) we found shows a completely different result. This study reports that botox induced complete hair growth in an alopeca totalis patient.
Overall, it seems that more studies are leaning towards the inefficacy of using Botox as a treatment of alopecia areata.
Highlights
- Botox is not effective for alopecia areata
- Periodic botox injections on forehead can lead to frontal hair loss
7. Azelaic Acid
Similar result to Anthralin treating alopecia areata
Azelaic acid is a popular ingredient used in various skin care products thanks to its scar / blemish fading ability. This is one of the reasons azelaic acid is used for a skin condition called rosacea.
Interestingly, one study shows that you may be able to use azelaic acid for hair loss (specifically for alopecia areata) as well.
This azelaic acid study included 31 alopecia areata patients. 15 subjects applied 20% azelaic acid while the rest (16) applied 0.5% anthralin cream topically for 12 weeks.
The result? It turned out the response rate for azelaic acid was almost as good as anthralin (53.3% vs 56.2%) for inducing hair regrowth
You can read more about azelaic acid for hair loss here.
Highlights
- Azelaic acid shows similar result to anthralin topical solution for treating alopecia areata in one study
8. Carboxytherapy
Successful, but with a slight relapse
Carboxytherapy is widely used for cosmetic purposes for removing stretch marks, cellulite and dark circles under eyes. It works by increasing blood circulation and restoring collagen levels.
A 2018 study (59) notes that carboxytherapy is effective for treating both alopecia areata and androgenetic alopecia. With a total of 80 participants, the researchers observed significant emergence of hair regrowth in both groups.
However, there were slight relapses following the treatment.
Finally, in order to maintain hair regrowth results, a minimum of 6 sessions are required.
Highlights
- One study treated androgenetic alopecia and alopecia areata participants successfully with carboxytherapy
- A slight relapse occurred after the treatment stopped
9. Hydroxychloroquine
Confusing results
Hydroxychloroquine (brand name: Plaquenil) is an oral antimalarial and anti-inflammatory drug used to treat malaria, lupus, and rheumatoid arthritis.
One study notes that hydroxychloroquine provides a wide range of immunomodulatory effects, thus also helping with pro-inflammatory cells reacting to hair follicles in alopecia areata.
There are only 3 studies using hydroxychloroquine for alopecia areata and they have very confusing outcomes (the hair regrowth response rate from each study: 0%, 55%, and 100%).
Here are before and after photos of a patient on Hydroxychloroquine (Plaquenil). The after photo shows positive progress:
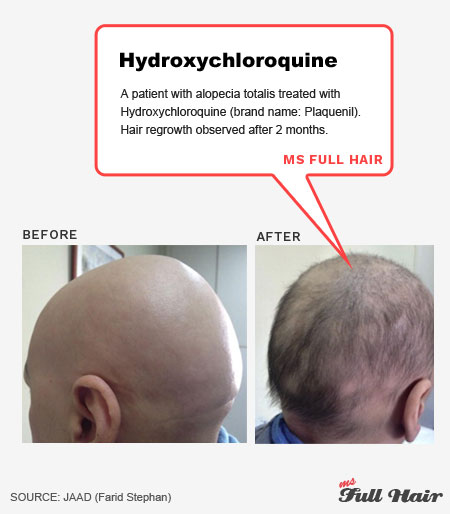
Hydroxychloroquine for frontal fibrosing alopecia:
Hydroxychloroquine therapy appears to be more popularly used to treat frontal fibrosing alopecia than alopecia areata (at least for now).
Frontal fibrosing alopecia is a type of scarring hair loss where frontal hairline shows visible thinning with recession. A number of studies note that hydroxychloroquine can be effectively used for treating this symptom.
The most common side effects include gastrointestinal intolerance, headaches, skin rash, loss of appetite and weight loss.
Highlights
- Each study shows a complete different response using Hydroxychloroquine for alopecia areata. This makes the true efficacy confusing
- Hydroxychloroquine appears to be more effective for treating frontal fibrosing alopecia than alopecia areata.
10. Inosiplex
Doesn’t look bad
Inosiplex, also known as isoprinosine or inosine pranobex, is an immune-stimulant drug.
While the exact mechanism of Inosiplex for alopecia areata is still unknown, it’s believed to work by regulating T cell mediated immune responses.
Several studies note that oral inosiplex shows effectiveness on alopecia areata, alopecia totalis and alopecia universalis patients.
A 2006 study (60) which involved 23 alopecia areata participants states that inosiplex showed considerable efficacy with 33.3% showing complete hair regrowth and 53.3% with partial regrowth.
One actual user we came across from Alopecia World (61) writes that inosiplex didn’t do much even after 4 months of consistent use.
Highlights
- Studies show decent success rates of using Inosiplex for alopecia areata
- One actual user says it didn’t induce any hair regrowth
11. Cryotherapy
Promising with minimal side effects
Cryotherapy, also known as liquid nitrogen cryotherapy therapy, is a trending new therapy which uses freezing temperatures as an inflammation-reducing remedy.
The theory behind it is to utilize cold temperatures to freeze off (or kill) harmful cells including cancer cells, lesions, and warts. While it’s considered to be safe, it’s still very new to the medical industry.
A number of studies we found show positive results of using cryotherapy for alopecia areata. Response rates for complete hair regrowth ranged from 23% to 62.5%.
Cryotherapy vs topical steroid for alopecia areata:
A 2013 study (62) compared cryotherapy with a conventional alopecia areata treatment:
- Group 1: Cryotherapy (as superficial cryotherapy therapy on the scalp)
- Group 2: Betamethasone lotion (topical steroid medication)
There were a total of 40 progressive and recalcitrant alopecia areata participants totalling 120 bald patches on the scalp.
Interestingly, both groups showed similar results: about 25% of participants from each group experienced 75%+ hair regrowth on the scalp).
However, there was a noticeable difference in relapse rate: people treated with cryotherapy experienced lower recurrence (41%), while 68% of topical betamethasone participants relapsed after the treatment.
All the studies we came across showed impressive success rates with minimal side effects.
Here are the comparison photos of using cryotherapy for alopecia areata from another study:
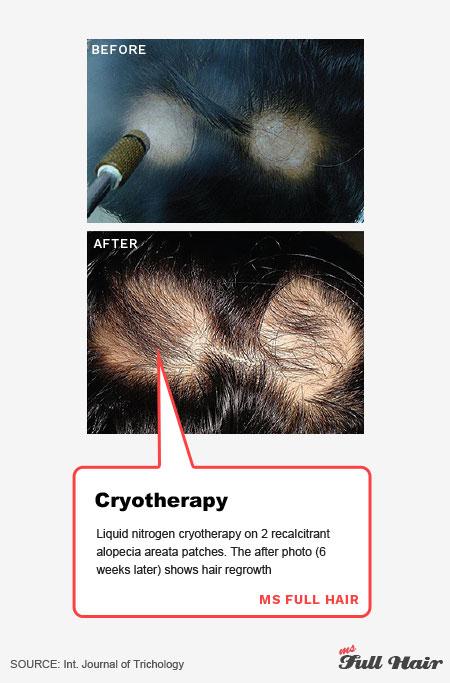
Highlights
- One study reveals that cryotherapy can be a good alternative to topical steroids for treating alopecia areata
- Minimal side effects were observed
12. Dapsone
Don’t bother
Dapson is a medicine with antibiotic, antibacterial, and anti-inflammatory properties.
Oral Dapson medicine is used for treating severe conditions such as dermatitis herpetiformis (chronic blistering skin condition) and leprosy (chronic bacterium infection damaging skin and nerves), while topical dapson is used for treating somewhat more mild symptoms such as acne.
For alopecia areata, a couple of research studies reveal that the treatment is NOT worth the risk.
A 1995 study (63) demonstrated that dapson is far inferior than topical immunotherapy and the success rate was about the same as the spontaneous hair regrowth rate.
Severe side effects:
Another study (64) reveals that more than half (54%) of the patients had to stop the treatment due to side effects such as significant malaise.
Highlights
- Dapsone is not worth the risk due to severe side effects
13. Topical retinoids
Savior or enemy?
Bexarotene and tretinoin are frequently used topical retinoids for treating alopecia areata in studies. Both are available via prescription, while adapalene gel (brand name: Differin gel) and topical retinoid are available over the counter.

The success rate for significant hair regrowth ranges from 12% to 71%, which is widely different.
Encouraging better absorption:
A couple of studies note that when retinoids (both studies used tretinoin retinoid) were used in conjunction with other therapies such as minoxidil or topical corticosteroids, the success rate for inducing hair regrowth dramatically went up.
For instance, a 2017 study experimented the efficacy of adapalene by randomly dividing 20 alopecia areata patients into two groups:
- Group A: Mometasone furorate cream (topical corticosteroids) with adapalene gel (topical retinoid)
- Group B: Mometasone furoate cream alone
Via evaluation of both groups in every 4 weeks, the researchers observed that group A (duo-therapy group) always had higher percentages of hair regrowth than group B (mometasone furoate alone) in each evaluation session.
Can topical retinoids also cause hair loss?
While alopecia areata studies on topical retinoids show promising results, some people are experiencing something totally opposite: hair loss.
We came across various posts on forums reporting that Differin gel (adapalene) appears to be the cause of excessive hair shedding.
In fact, a 2005 study (65) provides evidence for retinoid induced hair loss with the evaluation of cultured hair follicles. The researchers observed that retinoic acid (tretinoin) triggers upregulation of TGF-beta2 in derma papilla, which then induces a catagen-like (hair resting) phase in hair follicles.
Highlights
- Studies show that topical retinoids help with better absorption when used with other alopecia areata treatment
- Some people report excessive hair shedding after using topical retinoids such as Differin and Retin-A Micro
14. Simvastatin / ezetimibe
Various results
Simvastatin is a FDA-approved statin (lipid-lowering drug) that increases HDL (good cholesterol) and decreases LDL (bad cholesterol) by reducing the cholesterol made from the liver. Simvastatin has been used for treating heart disease, diabetes, and stroke.
Simvastatin also has immune response modulating effect.
Treatment of alopecia areata with simvastatin / ezetimibe:
A 2017 study (66) shows that when Simvastatin is used with Ezetimibe (a drug that decreases cholesterol absorption in the body), it creates synergistic effects for treating alopecia areata by inhibiting pro-inflammatory cytokines including IFN-y, TNF-a, IL-6, and IL-1B, in which all contribute to non-scarring hair loss.
Similar to other treatment, the hair regrowth results for simvastatin / ezetimibe for alopecia areata vary from 0% to 74%.
One study (67) notes that 24% of patients all experienced myalgia (muscle pain) during the treatment.
Highlights
- Similar to some of the other treatments, success rates for simvastatin/ezetimibe vary, but are more on the “ineffective” side
15. Low-dose naltrexone (LDN)
Reviews from actual users
Can LDN reverse hair loss? Naltrexone is an oral drug that was originally used for opioid addiction, but is also used for treating various autoimmune diseases at low dosages.
Low dose naltrexone (LDN) works by normalizing the immune system by increasing anti-inflammatory and decreasing pro-inflammatory cytokines.
Lots of Hype, but what about results?
While we haven’t found any alopecia areata study on LDN, there is a lot of interest about this treatment in some hair loss communities because it’s supposedly affordable and shows minimal side effects compared to other alopecia areata treatment.
But when it comes to actual results, it doesn’t seem to be so promising.
One user from a forum (68) mentions that she tried LDN for 1 year, but noticed very little hair growth. Making it even worse, she experienced a complete relapse right after discontinuing the medication.
One Reddit user (69) mentions that she used LDN for 7.5 months, but hasn’t seen any progress. Her doctor told her that unless she cuts dairy and gluten, it wouldn’t be very effective.
LDN side effects:
Some of the side effects for LDN include depression, headache, increased heart rate, severe anxiety and insomnia with long-term use.
Highlights
- Some actual users say it didn’t do anything to hair growth
16. Topical calcipotriol (Topical vitamin D)
Helps with hair regrowth
Calcipotriol is a synthetic form of vitamin D used to treat psoriasis by modulating excessive skin cell production.
Lack of vitamin D = alopecia: Recent studies reveal that levels of vitamin D are lower in people with alopecia areata as well as various autoimmune diseases.
High success rates of using topical calcipotriol (topical vitamin D) for hair regrowth:
Out of 4 studies that used topical applications, 3 studies indicate topical calcipotriol (vitamin D) induced hair regrowth in alopecia areata participants. All of the studies also show high success rates ranging from 59.1% (22 participants), 69.2% (48 participants), and 100% (1 participant).
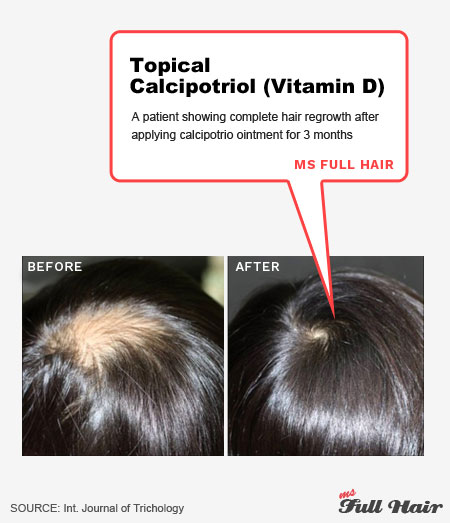
The one study which observed no significant hair regrowth used topical calcipotriol in combination with a scalp sensitizer.
Mild side effects:
Some mild side effects include dry and irritated skin, rash, and itching. The treatment is considered to be safe and well tolerated.
Highlights
- Studies observed alopecia areata participants with low levels of vitamin D
- Success rates of using topical calcipotriol are high
17. Topical triiodothyronine (thyroid hormone)
No significant difference
Triiodothyronine is a T3 thyroid hormone.
It’s well established that thyroid disease is one of the main causes of hair loss (especially diffused thinning hair) in women. A number of studies back up this claim by demonstrating that thyroid hormone receptors are expressed in hair follicles.
Promising mice study, but poor results in human studies:
When a group of researchers applied topical T3 on mice, increases in dermal thickening, epidermal proliferation, and hair regrowth were observed by depending on the dosage. The greater the dose, the better the results.
However, the success didn’t seem to translate well with human participants.
2012 study (70) involving 10 alopecia areata participants tested the efficacy of triiodothyronine ointment by applying it twice daily for 12 weeks.
The result? No significant difference.
This may be an indication that while thyroid hormone plays a crucial role in normal hair growth, there’s limited efficacy when used in topical form. More studies will be needed.
Highlights:
- Thyroid hormone plays an important role in healthy hair growth
- Topical form of thyroid hormone doesn’t appear to be effective for treating alopecia areata patients according to one study
18. Topical nitrogen mustard
Mixed results + few studies
Topical nitrogen mustard, also known as topical mechlorethamine hydrochloride, is an alkylating agent and skin irritant used to treat mycosis fungoide in a topical form.
There are only two studies on topical nitrogen mustard with mixed results.
The first study (71) from 1985 indicates that topical nitrogen mustard stimulated terminal hair regrowth in 7 out of 11 alopecia areata and alopecia totalis patients
However another research (72) from 2003 reports that only 1 out of 6 benefited from the treatment.
Highlights
- Topical nitrogen mustard shows mixed results in treating alopecia areata
- There are only 2 published studies on this treatment
19. Prostaglandins analogs
For eyelash alopecia
Prostaglandin is commonly used for the treatment of glaucoma (optic nerve damage due to increased pressure).
Bimatoprost (also known as Latisse) and latanoprost are the two most common topical prostaglandin analogs.
While most studies we found were limited to alopecia in eyelashes, there is one study that used Bimatoprost for scalp-related alopecia areata symptoms.
The researchers from the study (73) divided 30 alopecia areata participants into two groups and applied the following solution twice a day on the scalp for 3 months:
- Mometasone furoate cream (topical corticosteroid solution)
- Bimatoprost solution (prostaglandins analogs)
The result? The group that applied bimatoprost had “significantly better results” in terms of speed of the response, hair regrowth, as well as less side effects.
Highlights
- Prostaglandins analogs are widely used for alopecia in eyelashes
- There is only one study using it for scalp and it showed much greater response than topical corticosteroid
20. Imiquimod
Not effective
Imiquimod is a topical immune response modulator that stimulates cytokine production and activities. It’s used to treat genital warts.
When tested for alopecia areata, 3 out of 4 studies conclude that imiquimod didn’t have much effect on inducing hair regrowth.
Highlights
- Using topical imiquimod cream for alopecia areata shows poor response
21. Stem cell therapy
Very promising despite of a limited number of studies
Even though stem cell therapy has been widely used in treating various diseases and conditions, the number of studies used for hair regeneration / stimulation are still limited.
Here are studies we have found so far using stem cell as alopecia areata treatment:
Stem cell for AA study #1:
A 2015 Chinese study (74) notes that stem cell educator therapy effectively promoted hair regrowth among severe alopecia areata participants (patchy alopecia areata, alopecia totalis and alopecia universalis) without any significant adverse effects.
Through biopsies, the researchers found multiple positive signs for relieving alopecia areata symptoms which included:
- Balance in Th1/Th2/Th3 cytokine production
- TGF-B1 (transforming growth factor beta 1) around hair follicles, thus preventing autoimmune reaction
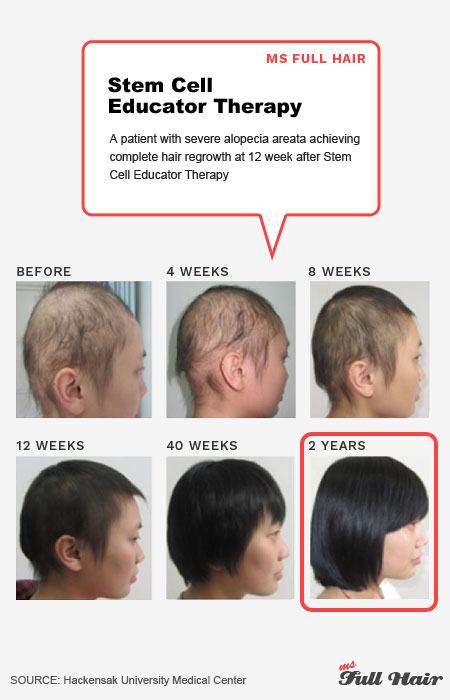
Stem cell for AA study #2:
Another study including 20 alopecia areata and 20 androgenetic alopecia subjects (total 40) reported significant improvement in both groups with just a single injection of autologous stem cells.
There were no side effects in this study as well.
Stem cell for AA study #3:
This research used adipose-derived stromal vascular cells (harvested from fat cells) in 20 alopecia areata patients.
The result? 100% participants experienced hair regrowth.
All of the stem cell studies so far have shown promising results in both efficacy and safety departments.
Highlights
- Studies show promising results and no side effects of using stem cell therapy for alopecia areata
- More studies will be needed
Ms Full Hair final thoughts
Are there alopecia areata treatments that work?

By now, you are probably waiting for the most important question: ‘So, what is the best treatment for alopecia areata (or alopecia totalis or even alopecia universalis)?’
Well, after analyzing hundreds of research studies, the answer (as expected) is not straightforward.
It’s very similar trying to find the best hair loss treatment for androgenetic alopecia. As we all know, there is no single solution that cures all male and female pattern hair loss (even the FDA-approved minoxidil is far from stimulating hair regrowth for all users).
In the same way, we couldn’t find an alopecia areata treatment that works for a majority of individuals in a large scale study.
HOWEVER, we will give you some takeaways and provide an overall summary on alopecia areata treatment. Although we can’t give you an ultimate answer for the best medicine for alopecia areata that works for everyone (because there isn’t one), this guideline will shed some light into the right direction.
- Treat it right away: The faster you treat alopecia areata, the higher chance you will have full recovery
- Spontaneous remission happens
- Alopecia areata recovery time: It really depends on the type of treatment used. For instance, intralesional corticosteroid injection (aka steroid shots) can induce hair regrowth in as early as 3 weeks. But minoxidil, on the other hand, will take at least 3-4 months to see results. On average, most treatments take at least 1 month for noticeable hair regrowth on bald spots (plus time and patience).
- Can alopecia be reversed? Some medications demonstrated full hair regrowth in some participants; however, relapse is the biggest issue in those medications as well. In other words, if you stop the treatment, there’s a very high chance that your hair will fall out again. This is especially true for most immunosuppressant drugs such as cyclosporine, sulfasalazine, and many others.
- Long term side effects: This means that if you want to maintain hair regrowth, you may become dependant on the working drug. As research has shown, the side effects of long term use can be dangerous in some cases.
- Emerging treatment: JAK inhibitors are the leading therapy many researchers have been actively working on. There are currently 3 JAK inhibitors that are regularly discussed in alopecia areata studies: Ruxolitnib (Jakafi), Tofacitnib (Xeljanz), and Baricitinib (Olumiant). The right dosage and adverse effects of long term uses are under investigation for various hair loss types: alopecia areata, alopecia totalis and alopecia universalis.
- Alopecia areata treatment with decent results: if your bald patchy hair loss is resistant to conventional treatments, look into the following therapies.
- If you are searching for topical corticosteroids for alopecia areata, look into betamethasone valerate foam. One study shows 2.3X more participants had hair regrowth using betamethasone valerate foam compared to betamethasone dipropionate lotion (61% vs 27%).
- Excimer laser therapy seems to give decent hair regrowth results and is also safer than other light therapies such as PUVA and NB UVB.
- Oral cyclosporine shows a significant response rate, but relapse also seems very common once the treatment stops.
- Alopecia totalis and alopecia universalis treatment with decent results: if you are suffering from alopecia totalis or alopecia universalis, you are probably aware of the fact that it’s difficult to induce hair regrowth. The more severe your hair loss becomes, the more resistant it is to most treatments. This explains why many dermatologists often recommend multiple therapies concurrently. Some of the studies that showed somewhat decent results include:
- Excimer laser therapy: Same reason as above
- Methotrexate: A number of studies note that methotrexate alone shows decent success rates in stimulating hair regrowth in severe alopecia, but one study notes that continuous treatment is required to avoid a relapse
- PUVA therapy: A couple of studies note that PUVA therapy showed significant response rates in severe alopecia areata, but some patients relapsed once the the therapy stopped. Also look into PUVA-turban therapy for fewer side effects.
- JAK inhibitors: Xeljanz appears to be regularly discussed in forums and shows encouraging before and after results; however, the optimal strength and safety are still two main concerns (and under investigation).
Now it’s your turn!
Have you tried any of these alopecia areata treatments? Share what you’ve tried so far and had success (or didn’t work) in the comment section below.













Wow! Amazing article. Thanks so much for putting all of this information into one place!
Great post about AA. Thank you so much!
The most informative article on AA I have seen. Having tried various treatments with some positive results the condition always returns. I have used a laser comb with positive results, however, having been very sick with another autoimmune condition last year I lost a lot of hair. My doctor is not interested in the condition and seeing a dermatologist where I live is next to impossible. I now use a hairpiece that covers my bald spots and have given up on a cure!
Has anyone tried Xeljanz (JAK inhibitor)? Any noticeable side effects?